Great new!! I finally successfully completed a full fitting from scratch using In-Situ testing. I found quite a bit of difference in the profile compared to what the audiologist got. Here is the comparison, grey line is the audiologist's test results. Colored line is from my in-situ test.
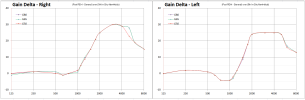
I proceeded to recalculate the gains after setting the preferences and running feedback adjustment. It was important to play the audios in preferences to decide the choices. I would have picked differently without listening. Here are the results comparing the gain numbers with what the audiologist had in the hearing aids before. That has gone through several adjustments since the original hearing test, and I was still very unhappy with the results.
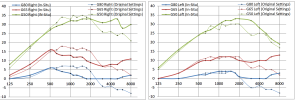
Note the drop in gain from 750-2500Hz on the right and pickup in gain for G50 above 2000Hz. I experienced no more annoying clanging of dishes in the kitchen and I can understand my wife's voice much better. She no longer sound tinny and cracky. I still have a major drop in gain above 3K Hz on the left ear due to feedback pushdown. I think I need to get new molds made to improve the feedback so that I can hear better with improved gains above 3K.
Since my profile is kind of flat with even loss across the frequencies, I disabled the frequency compression that shift higher frequency sounds down to lower frequencies like the audiologist had done. I think that also helped with my speech recognition. Definitely makes music sound better. I now can listen to the TV without 100% dependency on subtitles. Will venture out tomorrow into noisy environments and see how that works.
So grateful for all the help I got from this forum. Thank you.
I proceeded to recalculate the gains after setting the preferences and running feedback adjustment. It was important to play the audios in preferences to decide the choices. I would have picked differently without listening. Here are the results comparing the gain numbers with what the audiologist had in the hearing aids before. That has gone through several adjustments since the original hearing test, and I was still very unhappy with the results.
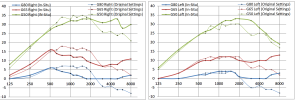
Note the drop in gain from 750-2500Hz on the right and pickup in gain for G50 above 2000Hz. I experienced no more annoying clanging of dishes in the kitchen and I can understand my wife's voice much better. She no longer sound tinny and cracky. I still have a major drop in gain above 3K Hz on the left ear due to feedback pushdown. I think I need to get new molds made to improve the feedback so that I can hear better with improved gains above 3K.
Since my profile is kind of flat with even loss across the frequencies, I disabled the frequency compression that shift higher frequency sounds down to lower frequencies like the audiologist had done. I think that also helped with my speech recognition. Definitely makes music sound better. I now can listen to the TV without 100% dependency on subtitles. Will venture out tomorrow into noisy environments and see how that works.
So grateful for all the help I got from this forum. Thank you.